Basic HTML Version













10 |
drinkanddrugsnews
| March 2014
Make It Happen! |
Service user conference 2014
Morning Panel
www.drinkanddrugsnews.com
‘S
cripts should be available whenever anyone needs them – if the recovery
message in local areas is about time-limiting, then that needs to be
changed,’ stated
Pete Burkinshaw
of Public Health England (PHE) in the
morning’s second session.
Chaired by service user coordinator
Alex Boyt
,
Challenges to making it happen
saw a panel of speakers discussing questions sent in by
DDN
readers. The first of
these was, ‘When the NTA’s responsibilities were merged into PHE we were
promised that recovery would be inclusive, but in our local area funding seems to
be only for abstinence-based services. What’s the future for those on scripts?’
Kirstie Douse
, head of legal services at Release and
DDN
’s legal columnist, told
the conference that it had been her experience that people were being ‘forced to
detox and reduce much faster than they would like, and that’s completely
unacceptable’. Forced recovery was a ‘quick route to relapse’ added Bob Campbell
of Phoenix Futures, while Birmingham GP
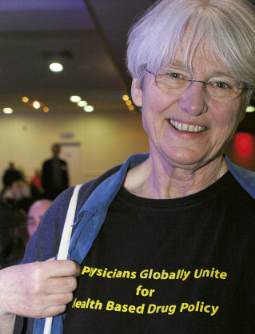
Dr Judith Yates
told the conference that,
‘we know methadone works for most people. There’s no one in the higher-ups
that’s advocating time-limited treatment.’ Service user activist
Anna Millington
,
however, stressed that ‘a lot of it is passive aggressive – being made to feel guilty
about staying on methadone is just as bad as being forced.’
‘There is an incentive to get people off scripts,’ stated one delegate. ‘It’s called
payment by results,’ while
Bob Campbell
stressed that, ‘like anything, it’s all about
short-term measures. There’s no investment in people’s futures.’
*****
The second question for panellists was, ‘In my area there’s only one GP who will
see patients with drug problems. This is disgraceful. Why is it treated differently
from any other illness?’
Services were not possible without some level of funding, said Judith Yates,
and it was now down to people in local areas to campaign for them. Despite all of
the arguments for shared care, however, drug treatment was ‘big business’ and
increasingly in the hands of large organisations, said Kirstie Douse. ‘Unfortunately,
that’s the direction it’s moving in.’
‘When I started in 1986, 0.2 per cent of general practice was looking after people
who had problems with drugs and alcohol,’ said retired GP and former DDN
columnist,
Dr Chris Ford
. ‘By 2011, the last year the figures were compiled, that had
risen to 32 per cent.’ Part of that had been the result of service user advocacy, she
stressed, but the field had entered ‘a period of chaos’ now. ‘How can people get care
when their organisation is just going into tender or just coming out of tender? We
need specialist care, and we have to stand up and be counted. We need to stand
together, wherever you are on the spectrum – drug-free or using every day.’
‘If you want the services, do it yourself, love,’ said one delegate. ‘At Lancashire
User Forum we did, and we’re massive.’
*****
The session’s final question was on alcohol. ‘As it causes more harm to more people
than drug use, why aren’t treatment resources allocated proportionately?’
panellists were asked.
There was no doubt that funding should be distributed proportionately, said
Pete Burkinshaw
. ‘I’m not arguing with that at all. But there seems to be a feeling
of Newtonian Law developing around commissioners – that if you invest in
alcohol then you need to disinvest in drugs.’
Funding for drug treatment was ten times that for alcohol, the session heard,
while the government had also abandoned its plans to introduce minimum pricing.
‘The alcohol industry is a multi-million pound industry,’ said one delegate. ‘It’s like
the Taliban or the Medellin Cartel having an influence on government policy.’
‘The only time money is given to drug treatment is when it affects mainstream
society – the HIV crisis, crime,’ said another. ‘Now that crime is going down,
what’s going to happen?’
‘There’s absolutely no distinction between drugs and alcohol,’ stated Pete
Burkinshaw at the session’s end. ‘We’re seeing more and more completely
integrated services. It’s totally down to local areas.’
The focus of the morning’s panel discussion was the ‘challenges to making it happen’
‘...being made
to feel guilty
about staying
on methadone
is just as bad
as being forced.’
ANNA MILLINGTON
Facing the challenge

