Basic HTML Version





In the mid ’80s
, when I found a prescribing doctor who would take me
on, I got offered the short or long script, reducing over two or six weeks. After
a detox that largely consisted of hugging the radiator in my cell, I got out of
jail in 2004 and found myself begging methadone off people because I was
told the waiting time for medication was the best part of a year. A few
months later, I was kicked out of my next rehab and got caught up in user
involvement. I was so impressed to find the treatment system had woken up,
people got the medication they needed, pretty much when they needed, and
often at the right dose.
Imagine all those people who no longer had to stand withdrawing on street
corners in the winter, hoping the dealer would take £9.40 instead of tenner,
because that’s what they had left after selling their coat and making the
phone call. Imagine all those people who wouldn’t have to inject all the wrong
crushed up pills and dried blood clots from old works just to get a brief
respite from endless withdrawals gnawing at their spirit.
So this was all ticking along nicely. Perhaps some people were getting
stuck on methadone and other options were not being explored. But when the
push for recovery began to take hold, a number of the people I knew on
substitute prescribing started getting nervous. They no longer felt safe: ‘Every
time I see my drug worker, we have a conversation about reducing my script.
Seeing him used to feel like support – now it just feels like pressure.’
Sure I was in recovery now, however you happened to measure it, and so
were a few people I knew and liked. But my personal sense of duty was still
fighting for those who didn’t have the strength, the desire or ability to face the
years of neglect, abuse, trauma or the harsh distress of unmedicated reality;
those who just needed to be held without judgement by a system of care.
*****
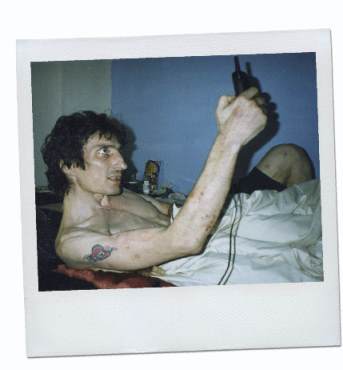
I know from my own experience
that pressure to embrace recovery
can work for some, but I also know that there are many for whom recovery,
especially in its abstinent form, is just too painful, difficult or unattractive. For
this lot, often those most at risk from death and disease, the recovery agenda
Could the recovery agenda be
killing people?
Alex Boyt
makes
the case from his own experience
makes services less relevant and safe. People who used to be held by the
treatment system are now confronted by goals for integrating into society the
moment they make it through the door. I am close to people who won’t even
consider engaging under these conditions – they’d rather take their chances
on the street, and I fear for their wellbeing. All too often they walk into a
service, already traumatised and deeply tired, only to be allocated a complex
ritual of recovery activities, usually with an implied or overt requirement that
prescribing is dependent on engaging.
When successful completions (often code for getting off your script)
became the focus, one of our local service managers said ‘we have to get
them in and out before we get to know them’. I regularly complained to
anyone who would listen that ‘only when crime and drug-related deaths go up
will policy-makers care that some of the most at risk are being failed by the
push for recovery.’ But somewhere inside I had retained a vestige of trust for
the treatment system and hoped that my concerns were misplaced.
However, when the drug-related death figures came out in September my
heart sank. I felt so angry, sad and disappointed: in one year a 32 per cent
increase in drug-related deaths and 20 per cent of that down to opiates. The
government says the cause was likely to be the increased strength of street
heroin, but the same stuff hits Wales where there was no increase in drug-
related deaths and recovery there is not the driving force it has become in
England. With the most at-risk engaging less, and those with their tolerance
lowered and facing their demons full on pushed too fast through the treatment
system, I worry for their wellbeing. I don’t claim to have proof, nor the ability or
will to interview the dead or the disengaged, but many I know share my belief
that aspects of the push for abstinence are dangerous.
The treatment system is of course largely a numbers game, and the need
to deliver targets is essential to keep the money flowing for any kind of care to
be delivered. I was at a presentation not long ago where the figures for those
completing treatment successfully were shown to vary in partnership areas
from about 4 per cent annually to 35 per cent. The figures indicate how
unhelpful some of the pressures for commissioners and service providers are.
What chance is there that the ideology from central government softens to
let people receive the care they need? You only have to note that the ACMD
were recently tasked by the Home Office to look at time-limited prescribing to
think the chances are slim. Is the recovery agenda killing people? You have to
think in places it probably is. My limited hope sits with the good people out
there still trying to deliver care in an increasingly harsh environment.
Alex Boyt works in central London as a service user coordinator
Staying alive
November 2014 |
drinkanddrugsnews
| 7
Opinion |
Recovery
www.drinkanddrugsnews.com
‘After a detox that largely
consisted of hugging the
radiator in my cell, I got out of
jail in 2004 and found myself
begging methadone off people
because I was told the waiting
time for medication was
the best part of a year...’

